Coronavirus and Construction
Designers Weigh Strategies for COVID-19 Isolation Rooms

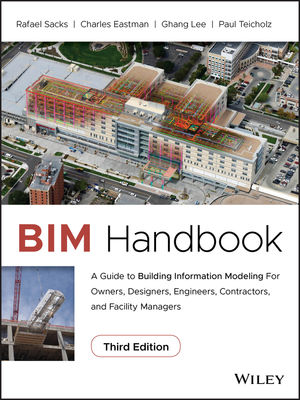
ASHRAE COVID-19 document offers various ways to manage air flow in an airborne infection isolation treatment room, using a mixing ventilation system strategy.
IMAGE COURTESY ASHRAE

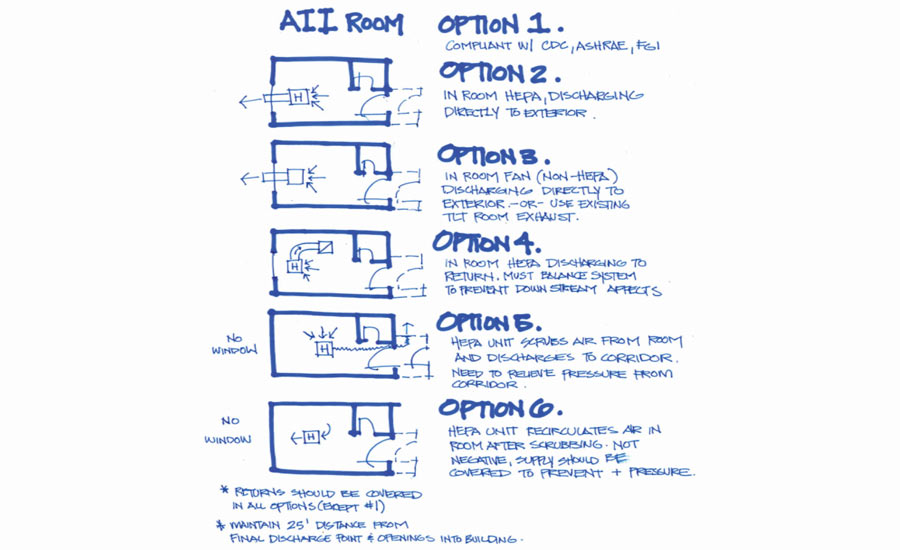
Mixing ventilation strategy most typically brings air into the room above the patient bed.
COURTESY RWDI

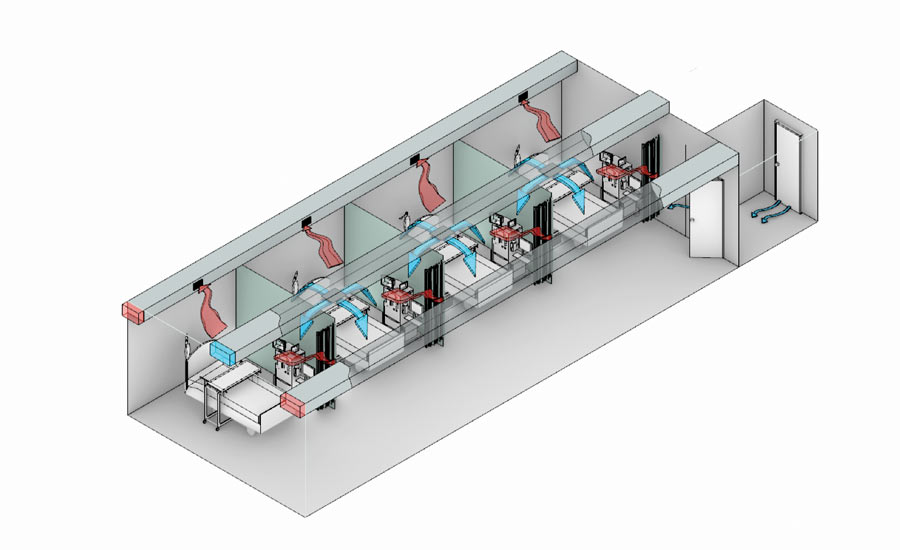
Displacement ventilation system with duct sock for supply air brings air into the room at the floor.
COURTESY RWDI

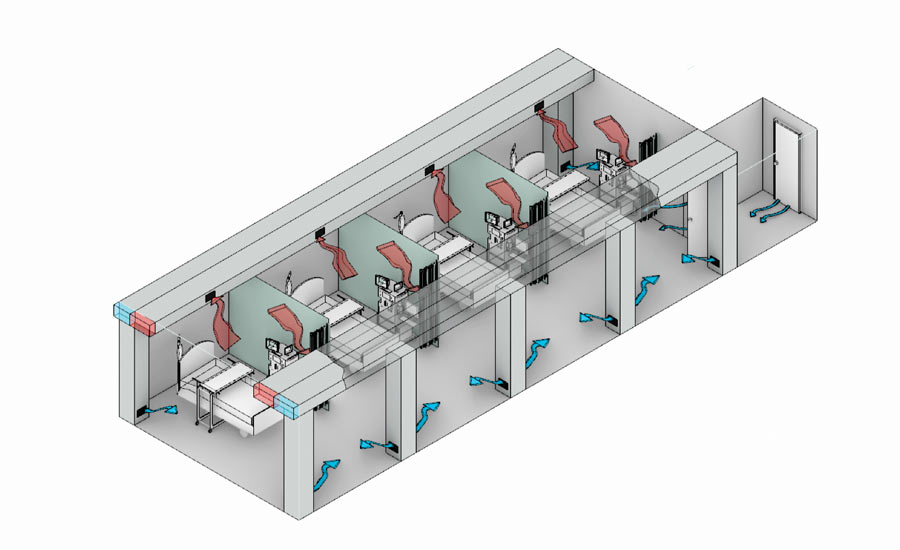
Displacement ventilation system with vents just above the floor.
COURTESY RWDI




While several teams have quickly set up COVID-19-related field hospitals in convention centers and places of public assembly—considered the low-hanging fruit of alternative sites for coronavirus surge beds—others are working behind the scenes on longer lead time retrofits and conversions for hospitals, hotels and dormitories. Many of these are aimed at increasing the supply of coronavirus patient intensive care units and airborne infection isolation rooms, with the goal of protecting health care workers from getting sick.
For the retrofits and conversions, health care architects and engineers are seeking the best ways to quickly design code-compliant and safe ICU and airborne infection isolation rooms, suites or wards, in a time of changing intelligence about virus transmission. The main reason for AII, rather than ICU-only rooms, is to keep health care personnel from contracting COVID-19.
For ENR’s latest coverage of the impacts of the COVID-19 pandemic, click here
“There is a subtle shift going on about how much transmission is occurring via droplets versus aerosols and in a health care setting, the concern about aerosols is higher because of the interventions, for example intubations, health care workers need to do to help the sick,” says engineer Duncan Phillips, a principal with RWDI, which designs AII rooms by, in part, modeling air flow through computational fluid dynamics (CFD).
Convention center pop-up hospitals, even those with some AII rooms, have been taking two weeks to a month to design, build and occupy. Even on the fast track, the more-complex ICUs or wards with all AII spaces could take one to six months, depending on variables. These include the project size and scope; the level of COVID-19 care; lead times for equipment; the original occupancy of the space; the need to convert the occupancy, which typically means upgrading fire alarm and life-safety systems; the permitting process; the locale; and more, say designers.
Collaboration Is Critical
For speed, many design firms are teaming up with contractors, in contractor-led design-build teams. Collaboration with owners, contractors, suppliers and users is critical to deliver the projects quickly. “Everyone is on the front lines, doing their parts,” says engineer Nolan Rome, U.S. health care director for WSP.
Help for fast-tracking the design of COVID-19 temporary treatment spaces is available from the American Society of Health Care Engineering, ASHRAE’s COVID-19 guidance document and from the American Institute of Architects.
For spaces other than convention centers and public assembly areas, there is more of a push toward ICUs than AII beds, says Timothy E. Krawetz, a health care senior principal for consulting engineer Syska Hennessy Group (SHG). Yet in the COVID-19 era, ICUs are starting to mimic AII rooms, though negative air pressure is not required by code for ICUs, he says.
A negative air pressure system directs air flow in a room through ventilation that generates pressure lower than the room’s surrounding air. Air naturally flows from areas of higher pressure to areas of lower pressure. In AII rooms, the air stays in the room, thanks to the negative pressure, and is exhausted mechanically.
There is no great mystery about the design of AII rooms or ICUs with AII. The pandemic has put pressure on the health care design and construction community to get the rooms designed, approved, built and operating quickly. The goal is to keep the designs simple so they can be deployed and maintained efficiently, with a minimum number of maintenance personnel, says Rome.
WSP is designing a temporary hospital in South Carolina. “We are thinking like facility operators instead of design engineers,” he says.
One obstacle is equipment lead time, which can vary from three to six months. There is a three- to five-week lead time for ventilators and a four- to six-month lead time for negative-pressure machines, says Kimberly R. Cowman, national director of engineering for Leo A Daly.
“There is a three- to five-week lead time for ventilators and a four- to six-month lead time for negative-pressure machines.”
-Kimberly R. Cowman, national director of engineering, Leo A Daly
There is 30-day delivery for hospital-grade air-handling units, says SHG’s Krawetz.
SHG is in the middle of a month-long ICU project—from start to finish—that involves gutting two residential floors, formerly for nurses, of a 17-story public hospital building in New York City. The client, partway through design, asked for the capability to switch the rooms to negative pressure. Part of the challenge is that the programs keep changing, mid-design, says Krawetz.
It took SHG 15 days, working 15 to 18 hours every day of the week, to produce the 66 drawings needed for the project. That design work would normally take six months, Krawetz says.
Construction is ongoing around the clock. Occupancy is expected by about April 15, says Krawetz.
For AII spaces, the goal is to manage all contaminants, in the form of gases or droplets, through air flow. Though larger droplets fall, potentially contaminating surfaces, smaller droplets will float and can be inhaled.
Mixing Ventilation System
The most common type of AII air-handling strategy is known as a mixing ventilation system or a mixing air-distribution system, says RWDI’s Phillips. Mixing typically delivers air into the upper level of the room and uses the momentum of the incoming air to distribute it around the room—mixing the clean incoming air and contaminants in the room as it does so. The exhaust duct, usually in the ceiling or behind the patient bed, extracts the mixed air and moves it through a HEPA-filter air purifier before releasing it either outdoors or into a corridor. The filter does not catch the COVID-19 virus but it catches particulates that trap the virus.
Phillips is against mixing ventilation because fresh air is contaminated and pollutants are stirred around the room. Instead, he advocates a displacement ventilation system, which minimizes mixing. DV delivers cooler air into the room low to the floor, through a perforated tube along the floor called a duct sock or through several vents along the floor.
DV works because the cooler ventilation air, warmed by occupants and equipment, lifts the contaminants as it rises. The fresh air does not mix as much with the contaminated air. Larger droplets will still fall to the floor and other surfaces because of the low speed of the rising fresh air.
Because the smaller aerosol droplets are light and track with air, they become stratified at the ceiling while the exhaust is pulling them from the room. This turns the upper layer of the room into a storage zone for the fine droplets above the occupied space, says Phillips.
Also, the exhaust at the ceiling level is able to extract the contaminants at a higher concentration because they were not diluted by the mixing, making that exhaust more effective.
Phillips says that the mixing approaches offered in guidance documents don’t describe how to deliver air into the room. Instead, they focus on how to extract air from the space.
“Everyone is on the front lines, doing their parts.”
-Nolan Rome, U.S. health care director, WSP
“You cannot properly control airborne transmission just by choosing how to exhaust from the room,” he says.
The exhaust has to be in the right place, but critically so does the supply, Phillips maintains. “Spending too much time worrying about the extraction is like trying to suck out a candle. You will only be successful once you have burned your lips,” he says.
Mechanical engineer Tariq Amlani, a buildings principal with Stantec, agrees with the general concept that DV can reduce the overall contaminate concentration in the room. But he cautions that though the directional air flow aspect of DV can help control the flow of contaminates within the space, the strategy is “highly reliant” on the location of the low-level supply grills and high-level exhaust grills.
Grill Locations
Using DV alone “may not help and can actually hurt infection control, if you don’t get the grill locations correct,” Amlani says. “DV or not, in consideration of the current COVID-19 situation, I don’t believe that there would be any differences in the personal protective equipment requirements for the health care workers in these spaces,” he adds.
Amlani is also concerned about keeping the duct sock sanitized. In addition, with DV there are limitations on how cold the supply the air can be without running into comfort issues.
A typical overhead ventilation system can have supply air as cool as 55° F without comfort complaints. With DV, you have a lower limit on your supply air temperature of approximately 65° F, as per the ASHRAE code, says Amlani.
There can be other concerns, he adds. DV relies on cool air “pooling” at the floor level and then “pluming” up as the cool air warms up at heat sources. “If you have a room with a window that can receive direct sunlight, this can be a significant problem,” adds Amlani.
Also, “if you have a room on the perimeter of the building and you are using DV, you will need a secondary decoupled heating system, such as radiant panels or radiant floors to offset envelope heat losses,” says Amlani. “This may not be practical to implement in all buildings and projects.”
Others agree that DV has potential, but only if properly executed. “There are unique challenges,” says Michael P. Sheerin, CEO of TLC Engineering. One is that the low-wall diffusers need to be routed in chases that take up valuable area in a patient room. And because the delivered air temperature is adjusted, it is different from the heating, ventilating and air-conditioning support to the interior spaces, he adds.
Sheerin concedes that the basic principles of DV—supply air diffusers at the entry and health care worker side of the patient bed and exhaust near the head of the bed—are “time-honored and a sensible means of encouraging a clean-to-less-clean airflow pattern in a space, especially important in an isolation space.”
Daly's Cowman agrees that while RWDI “makes a case for displacement ventilation, there are inherent design challenges with the layout of this type of system in practice.”
The location of the supply diffusers and the ability to keep the area in front of the diffusers clear of equipment would mandate an additional level of coordination with the architecture, equipment planning and hospital operators to ensure the design would perform as intended, says Cowman.
She suggests future research into the optimum design and distribution of air flow to serve patient isolation rooms to protect health care workers. “In all cases, there is value in thoughtful placement of supply and exhaust locations to move air from clean to dirty environments in the space,” she says.